Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
Scientific Reports volume 13, Article number: 22323 (2023 ) Cite this article Golf Umbrella

Mechanisms of coronary artery bypass grafting (CABG) and percutaneous coronary intervention (PCI) differ as CABG provides surgical collateralization and may prolong life by preventing future myocardial infarctions (MI). However, CABG benefits are unclear in octogenarians, where surgical risk is often perceived as higher and PCI is chosen more liberally. We performed a meta-analysis of studies comparing outcomes in octogenarians with left main or multivessel disease who underwent CABG or PCI. Primary outcome was late mortality (> 5 years). Secondary outcomes were perioperative mortality, MI, re-revascularization (R-R), acute renal failure (ARF), and stroke. Fourteen studies with 17,942 patients were included. CABG was associated with lower late mortality (hazard ratio, HR: 1.23, 95% confidence interval: CI 1.05–1.44, p < 0.01). In the pooled Kaplan–Meier analysis CABG showed significantly lower risk of death in the follow-up compared to PCI (HR: 1.08, 95%CI 1.02–1.41, p = 0.005). Landmark analyses confirmed the survival advantage of CABG over PCI after 21.5 months of follow-up (HR: 1.31, 1.19–1.44, p < 0.0001), but suggested advantage of PCI over CABG in the first 30-days (HR: 0.72, 0.64–0.82, p < 0.0001) and comparable survival from 1 to 21.5 months (HR: 0.98, 0.92–1.05, p = 0.652). We found lower risk for MI and R-R after CABG but higher perioperative mortality and no differences in ARF and stroke. CABG appears superior to PCI over time in octogenarians with complex CAD. This survival advantage is associated with fewer events of MI and R-R; however, it comes with an increased risk in perioperative mortality.
Ashish Sarraju & Steven E. Nissen
Mattia Arrigo, Mariell Jessup, … Alexandre Mebazaa
Alexander Zarbock, Mitra K. Nadim, ... Lui G. Forni
Recent data suggest that mechanisms of coronary artery bypass grafting (CABG) surgery and percutaneous coronary intervention (PCI) differ1. Guideline-conform PCI is focused on treating flow-limiting lesions, but the majority of myocardial infarctions occur at non-flow-limiting stenoses1. Thus, PCI cannot be expected to significantly limit new myocardial infarctions (MI). In contrast, CABG may do so by bypassing most coronary lesions providing downstream “collateralization” to the grafted vessel and possibly to other coronary arteries, which may prevent myocardial infarctions caused by ruptured plaque thrombosis or sudden progression of plaques that were not flow limiting at the time of surgery1,2. This potential mechanism was confirmed by a recent meta-analysis of all randomized studies comparing PCI and CABG, which showed that the observed survival advantage of CABG over PCI in randomized trials was associated with a significant reduction of spontaneous MIs in the surgical arm3.
As one ages, the likelihood of experiencing an acute MI progressively increases. In the United States, individuals aged 65 and older account for over 60% of all cases of acute MI, with approximately one third of cases occurring in those over 75 years old4. The mortality rates following an acute MI also increase significantly with age. This means that about 60% of all MI-related deaths in the United States occur among the 6% of the population aged 75 years or older4.
Due to the increased risk of MIs in octogenarians it might be well conceivable that surgical collateralization through CABG might be the superior invasive treatment. However, in those patients surgical risk is often perceived as prohibitively high and PCI is chosen more liberally. So far, there is no clear recommendation addressing the invasive treatment options for coronary artery disease in octogenarians. Therefore, in this analysis we set out to systematically review the literature on the impact of the invasive treatment modality on clinical outcome in octogenarians with coronary heart disease.
Ethical approval of this analysis was not required as no human or animal subjects were involved. This review was registered with the National Institute for Health Research International Registry of Systematic Reviews (PROSPERO, CRD42022345249).
We performed a comprehensive literature search to identify contemporary studies reporting short-, mid- and long-term outcomes between CABG and PCI in octogenarians with left main or multivessel coronary disease. Searches were run on June, 2022 in the following databases: Ovid MEDLINE (2008 to present); Web of Science (2012 to present); and The Cochrane Library (1993 to present). The search strategy for Ovid MEDLINE is available in Supplementary Table 1.
The study selection followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) strategy. After de-duplication, records were screened by two independent reviewers (TC and LR). Any discrepancies and disagreements were resolved by a third author (HK). Titles and abstracts were reviewed against pre-defined inclusion and exclusion criteria.
Studies were considered for inclusion if they were written in English and reported direct comparison between CABG and PCI in octogenarians with left main or multivessel coronary disease. Animal studies, abstracts, case reports, commentaries, editorials, expert opinions, conference presentations, and studies not reporting the outcomes of interest were excluded. The full text was pulled for the selected studies for a second round of eligibility screening. References for articles selected were also reviewed for relevant studies not captured by the original search.
The Risk of Bias in Non-Randomized Studies of Interventions tool (ROBINS-I) was systematically used to assess included studies for risk of bias5. The studies and their characteristics were classified into low, moderate and serious risk of bias. Two independent reviewers (TC and LR) assessed risk for bias. When there was a disagreement, a third reviewer (HK) checked the data and made the final decision (Supplementary Fig. 1).
Two reviewers (TC and LR) independently performed data extraction. Accuracy was verified by a third author (HK). The extracted variables included study characteristics (publication year, country, sample size, study design, mean follow-up, presence or absence from population adjustment and outcome definitions) as well as patient demographics (age, sex, mean left ventricular ejection fraction—LVEF, hypertension, diabetes, smoking status, prior cerebrovascular accident—CVA, prior myocardial infarction MI, prior PCI, renal failure and chronic obstructive pulmonary disease—COPD).
Primary outcome was long-term all-cause mortality defined by studies with follow-up > 5 years. Secondary outcomes were perioperative all-cause mortality (30-day/in-hospital), acute renal failure, myocardial infarction, re-revascularization and stroke.
We conducted meta-analyses to compare the outcomes of CABG versus PCI. Relative risks (RR) and 95% confidence intervals (CI) were calculated for each outcome. A RR greater than 1 indicated that the outcome was more frequently present in the CABG arm. Inherent clinical heterogeneity between the studies was balanced via the implementation of a random effects models. Results were displayed in forest plots. Between-study statistical heterogeneity was assessed with the Cochran Q statistic and by estimating I2. High heterogeneity was confirmed with a significance level of p < 0.10 and I2 of at least 50% or more. Publication bias was assessed via funnel plots and Eggers’ test for the primary outcome and p < 0.10 was considered statistically significant. Leave-one-out sensitivity analyses were also performed for the primary outcome. All analyses were performed using STATA IC17.0 (StataCorp LLC, College Station, Texas).
We used the methods described by Wei et al. to reconstruct IPD from the Kaplan–Meier curves of all eligible studies for the long-term outcomes6,7. Raster and Vector images of the Kaplan–Meier survival curves were pre-processed and digitized, so that the values reflecting to specific timepoints with their corresponding survival/mortality information could be extracted. Where additional information (e.g., number-at-risk tables or total number of events) were available, they were used to further calibrate the accuracy of the time-to-events. Departures from monotonicity were detected using isotonic regression and corrected with a pool-adjacent-violators algorithm6,7. To confirm the quality of the timing of failure events captured, we thoroughly checked the consistency with the reported survival or morality data provided in the original publications.
The Kaplan–Meier method was used to calculate the overall survival. The Cox proportional hazards regression model was used to assess between-group differences. For these Cox models, the proportional hazards assumption was verified by plotting scaled Schoenfeld residuals, log–log survival plots, and predicted versus observed survival functions. We plotted survival curves using the Kaplan–Meier product limit method and calculated the Hazard Ratios (HRs) and 95% CIs of each group. A HR greater than 1 indicated that the outcome was more frequently present in the PCI arm.
This work has been selected to be presented at the 103rd AATS Annual Meeting.
A total of 112 studies were retrieved from the systematic search, of which 14 met the criteria for inclusion in the final analysis. Figure 1 shows the PRISMA flowchart for study selection. Included studies were published between 1991 and 2021, all studies were observational cohorts, and 6 were multicentric. One study was multinational, 4 originated from the United States, 2 from Canada, 2 from Japan, and 1 each from England, Netherland, Finland, Italy and China.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram.
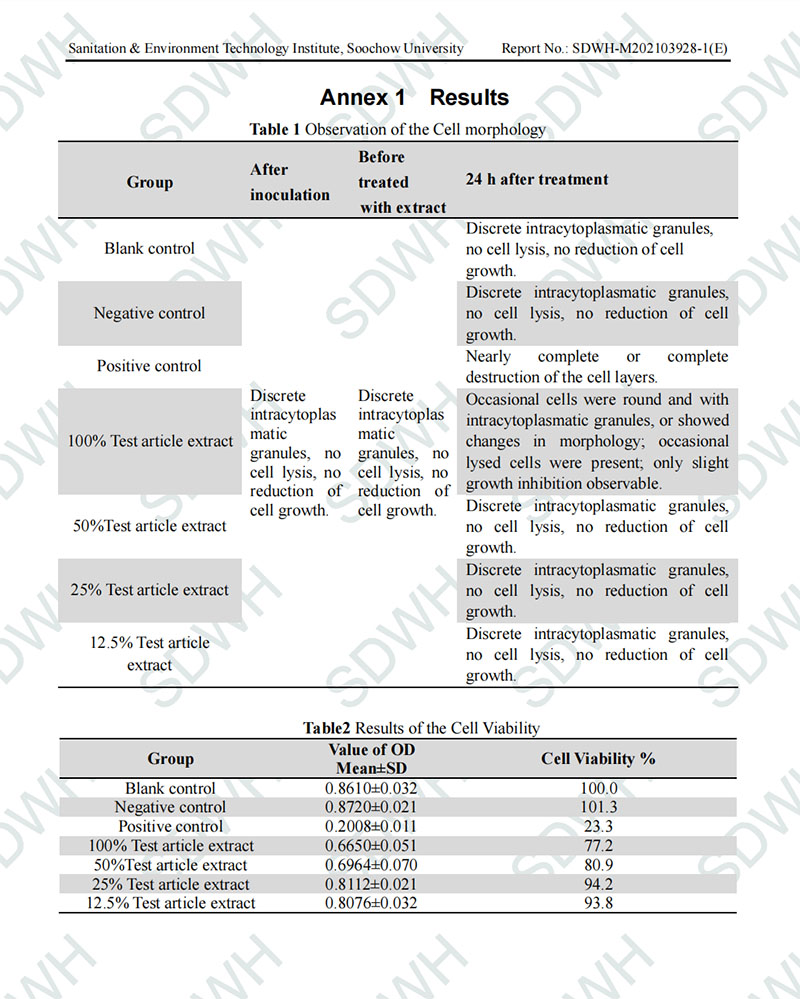
Tables 1, 2 shows the details of the included studies. Thirteen studies were based on risk-adjusted populations. A total of 17,942 patients were included in the final analysis. The number of patients in each study ranged from 128 to 10,141.
Supplementary Table 3 summarizes the demographic data of the patient population in each study. Percentage of female patients ranged from 22.7 to 71.4%; percentage of mean LVEF ranged from 48 to 60.6%; percentage of hypertension ranged from 26 to 90%; percentage of diabetes ranged from 14.6 to 93%; percentage of positive smoking status ranged from 3 to 34.9%; percentage of prior CVA ranged from 4.2 to 17.4%; percentage of prior MI ranged from 17.8 to 67.1%; percentage of prior PCI ranged from 7.8 to 17.4%; percentage of renal failure ranged from 1 to 13.5% and the percentage of COPD ranged from 2 to 18.9%. Supplementary Table 3 shows the specific description of the included outcomes.
Figure 2 and Table 3 outline the detailed results of the meta-analysis.
(Central Picture). Graphical abstract showing the main findings of the analysis.
Figure 3 shows the forest plot for long-term all-cause mortality. The patients who underwent CABG showed lower incidence of long-term all-cause mortality (HR = 1.23, 95% CI 1.05–1.44, p < 0.01).
Forest plot for long-term all-cause mortality. CI confidence interval, HR hazard ratio.
Supplementary Fig. 2 shows the leave-one-out analysis showing that most of the studies confirm the robustness of the analysis, with minimal variations of the confidence interval. Supplementary Fig. 3 provides the funnel plot for the publication bias assessment.
Supplementary Fig. 4 shows a sub-group analysis dividing studies according to the publication year. There was no significant difference between the two therapy groups in studies published before and after 2010 (p-interaction = 0.49).
Overall, 12 Kaplan–Meier curves were processed, digitalized, and reconstructed. A side-by-side comparison of our reconstructed Kaplan–Meier curves and those found in the original publications is provided in Supplementary Fig. 5. Using the previously described methodology, we extracted the IPD from these curves.
Figure 4 shows the pooled Kaplan–Meier curves of reconstructed IPD. Patients who underwent CABG had significantly lower risk of death in the follow-up compared to those who underwent PCI (HR: 1.08, 95% CI 1.02–1.41, p = 0.005).
Pooled Kaplan–Meier curves showing the cumulative risk of all-cause mortality following CABG and PCI. CI confidence interval, HR hazard ratio.
Violation of the proportional hazards assumption was observed between scaled Schoenfeld residuals and follow-up time, as well as in log–log survival plots (Supplementary Fig. 6). This indicated that the HR is not constant over time.
Since we observed that the proportional hazards assumption was violated, we proceeded with landmark analysis, designating 21.5 months (the point where both curves crossed in Fig. 4A) as the landmark timepoint.
Figure 4B shows the 30-day survival analysis, which suggested that PCI offers a survival advantage compared to CABG (HR: 0.72, 0.64–0.82, p < 0.0001).
Figure 4C shows the landmark analysis from 1 to 21.5 months, which suggested that the two techniques offer comparable survival outcomes compared (HR: 0.98, 95% CI 0.92–1.05, p = 0.652).
Figure 4D shows the landmark analysis after 21.5 months of follow-up, which revealed a statistically significant survival advantage in favor of CABG over PCI (HR: 1.31, 95% CI 1.19–1.44, p < 0.0001).
Supplementary Fig. 7 shows the forest plot for perioperative all-cause mortality. The patients who underwent CABG showed higher incidence of perioperative all-cause mortality (RR 1.21, 95%CI 1.07–1.36, p < 0.01).
Supplementary Fig. 8 shows the forest plot for acute renal failure. There was no significant difference between the two therapy groups (RR 1.21, 95%CI 0.54–2.72, p = 0.64).
Figure 5 shows the forest plot for myocardial infarction. The patients who underwent CABG showed lower incidence of myocardial infarction (RR 0.51, 95%CI 0.46–0.56, p < 0.01).
Forest plot for myocardial infarction. CI confidence interval, RR relative risk.
Supplementary Fig. 9 shows the forest plot for re-revascularization. The patients who underwent CABG showed lower incidence of re-revascularization (RR 0.31, 95%CI 0.22–0.45, p < 0.01).
Supplementary Fig. 10 shows the forest plot for stroke. There was no significant difference between the two therapy groups (RR 1.52, 95%CI 0.96–2.39, p = 0.07).
Our analysis suggests that for the treatment of octogenarian patients with left main or multivessel disease CABG is associated with significantly lower risk of death in the long-term follow-up compared to PCI (survival advantage after the first 21.5 months of follow-up). This superiority of CABG is associated with fewer events of myocardial infarction and re-revascularization. However, perioperative mortality is higher with CABG.
Our results are relevant as they provide valuable information, affecting the treatment of a substantial number of patients. Currently, there are aproximately 147 milion octogenarians worldwide, representing 1.9% of the global population8. This global number of octagenarians has risen significantly over the last decades and is projected to rise further. As age is the strongest factor connected with the development of coronary artery disease (CAD)9, this relates in millions of patients worldwide faced with a with a potential treatment choice between CABG or PCI. Necropsy studies for example, have demonstrated a high prevalence (∼ 60%) of obstructive CAD in patients ≥ 80 years of age, often with features of advanced disease [e.g., calcification (80% to 90%), multivessel disease (40%)]9,10. The prevalence of CAD (defined as coronary insufficiency, myocardial infarction, angina pectoris, or CAD-related death) in octogenarins was reported with 31.2% for the age group 85–89 by the Franmingham Heart Study and similar rates were observed by the Cardiovascular Health Study (30.9% for 80–84 years and 35.8% for 85–89 years)10.
In this context, one of the main findings of our work is the fact that the survival curves of CABG and PCI in octogenarian patients cross (similar to other known studies comparing CABG and PCI) after approximately 2 years.
Currently treatment recommendations and guideliens for CAD outlining when to recommend which treatment option (e.g., CABG or PCI) are mostly based on randomized trials, which are bound to reflect the average treatment effect for an often selected patient population11. Despite the huge number of octagenarians affected by CAD worldwide, they have been typically under-represented in randomized cardiovascular clinical trials as many studies have either excluded older patients or only included those at lower risk12. For example, the mean age of the randomized patients in the EXEL trial was 66 years13 and and 65 years in the FAME 3 clinical trial14. Thus our work may fill the evidence gap resulting from the underrepresentation of octogenarian patients in such trials, as it summarizes the current data and presents information not provided by randomized trials.
However, it is so far unknown if quality of life measures, functional status, and overall well-being also follow this trend. Understanding how these factors are affected by CABG or by PCI in octogenarians can provide valuable insights for personalized treatment recommendations and should be a matter of future research.
Our results, once again put center stage the question of the underlying mechanisms leading to and explaining them. As mentioned earlier, the concept of surgical collateralization might explain the life-prolonging (i.e., prognostic) effect of CABG, which appears to be due to prevention of future myocardial infarctions1. Our work once more confirms this concept, as the survival advantage for CABG was as expected associated with fewer events of myocardial infarctions and re-revascularization. This infarct-preventing mechanism through CABG collateralization might be also the explanation, why the long-term survival of elderly patients after CABG is superior to that of their age-matched population15,16.
CABG has always been considered the more invasive treatment option compared to PCI, and in octogenarian patients physicians have often been reluctant to recommend it, especially in cases with other comorbidities. However, in our analysis we did not find any significant difference in the rates of acute kidney injury and stroke between the groups. Furthermore, recent data has illustrated that generally CABG might be the superior treatment in patients with diabetes17 or chronic kidney disease18 and/or dialysis19. Thus, it seems that the treatment benefit of CABG does not diminish in patients of advanced age and/or comorbidities, and our results support that probability.
One of the main findings of our work is the fact that the survival curves of CABG and PCI in octogenarian patients cross (similar to other known studies comparing CABG and PCI) after approximately 2 years. However, it is so far unknown if quality of life measures, functional status, and overall well-being also follow this trend. Understanding how these factors are affected by CABG or by PCI in octogenarians can provide valuable insights for personalized treatment recommendations and should be a matter of future research.
Nevertheless, this information is essential as it may enable individualized approach in octogenarians- ones with clearly limited life expectancy might be be mor suiutable for PCI, but octogenarians with longer life expectancy should be informed about this trade-off between initial risk and survival advantage.
This is the first meta-analysis of reconstructed time-to-event data to address this important topic. Moreover, we analyzed 4 different outcomes besides mortality. However, this work has the intrinsic limitations of observational series, including the risk of methodological heterogeneity of the included studies and residual confounders. In addition, treatment allocation bias is likely present in all observational series comparing two therapies with different operative risk and invasiveness. Moreover, one study contributed significantly for the final sample size, which could contribute strongly for the final treatment effect.
The results support the concept that CABG provides a survival advantage over PCI for complex CAD over time even in octogenarians. This survival advantage is associated with fewer events of myocardial infarction and re-revascularization; however, it comes with an increased risk in the perioperative mortality after CABG. Since survival curves cross after approximately 2 years, octogenarians with longer life expectancy should be informed about this trade-off between initial risk and survival advantage.
The data underlying this article are available in the article and in its online supplementary material.
Doenst, T. et al. PCI and CABG for treating stable coronary artery disease: JACC review topic of the week. J. Am. Coll. Cardiol. 73, 964–976 (2019).
Doenst, T., Bonow, R. O., Bhatt, D. L., Falk, V. & Gaudino, M. Improving terminology to describe coronary artery procedures: JACC review topic of the week. J. Am. Coll. Cardiol. 78, 180–188 (2021).
Gaudino, M. et al. Difference in spontaneous myocardial infarction and mortality in percutaneous versus surgical revascularization trials: A systematic review and meta-analysis. J. Thorac. Cardiovasc. Surg. 165, 662-669.e14 (2021).
Article PubMed PubMed Central Google Scholar
Rich, M. W. Epidemiology, clinical features, and prognosis of acute myocardial infarction in the elderly. Am. J. Geriatr. Cardiol. 15, 7–11 (2006) (quiz 12).
Sterne, J. A. et al. ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. BMJ 355, i4919 (2016).
Article PubMed PubMed Central Google Scholar
Guyot, P., Ades, A. E., Ouwens, M. J. N. M. & Welton, N. J. Enhanced secondary analysis of survival data: Reconstructing the data from published Kaplan-Meier survival curves. BMC Med. Res. Methodol. 12, 9 (2012).
Article PubMed PubMed Central Google Scholar
Wei, Y. & Royston, P. Reconstructing time-to-event data from published Kaplan-Meier curves. Stata J. 17, 786–802 (2017).
Article PubMed PubMed Central Google Scholar
Nations U. United Nations world population prospects 2019. (2019).
Andrus, B. & Lacaille, D. 2013 ACC/AHA guideline on the assessment of cardiovascular risk. J. Am. Coll. Cardiol. 63, 2886–2886 (2014).
Madhavan, M. V., Gersh, B. J., Alexander, K. P., Granger, C. B. & Stone, G. W. Coronary artery disease in patients ≥80 years of age. J. Am. Coll. Cardiol. 71, 2015–2040 (2018).
Gaudino, M., Bagiella, E., Chang, H. L. & Kurlansky, P. Randomized trials, observational studies, and the illusive search for the source of truth. J. Thorac. Cardiovasc. Surg. 163, 757–762 (2022).
Lee, P. Y., Alexander, K. P., Hammill, B. G., Pasquali, S. K. & Peterson, E. D. Representation of elderly persons and women in published randomized trials of acute coronary syndromes. JAMA 286, 708–713 (2001).
Article CAS PubMed Google Scholar
Stone, G. W. et al. Five-year outcomes after PCI or CABG for left main coronary disease. N. Engl. J. Med. 381, 1820–1830 (2019).
Fearon, W. F. et al. Fractional flow reserve-guided PCI as compared with coronary bypass surgery. N. Engl. J. Med. 386, 128–137 (2022).
Diegeler, A. et al. Five-year outcome after off-pump or on-pump coronary artery bypass grafting in elderly patients. Circulation 139, 1865–1871 (2019).
Doenst, T. et al. Cardiac surgery 2019 reviewed. Thorac. Cardiovasc. Surg. 68, 363–376 (2020).
Wang, R. et al. Ten-year all-cause death after percutaneous or surgical revascularization in diabetic patients with complex coronary artery disease. Eur. Heart J. 43, 56–67 (2021).
Article PubMed PubMed Central Google Scholar
Yamamoto, K. et al. Percutaneous coronary intervention versus coronary artery bypass grafting in patients with versus without chronic kidney disease. Am. J. Cardiol. 145, 37–46 (2021).
Gaipov, A. et al. Predialysis coronary revascularization and postdialysis mortality. J. Thorac. Cardiovasc. Surg. 157, 976-983.e7 (2019).
Conrotto, F. et al. Long term outcomes of percutaneous coronary interventions or bypass grafting surgery for left main coronary artery disease in octogenarians: A DELTA registry sub-study. Eur. Heart J. 35, 970–970 (2014).
Dacey, L. J. et al. Long-term survival after surgery versus percutaneous intervention in octogenarians with multivessel coronary disease. Ann. Thorac. Surg. 84, 1904–1911 (2007) (discussion 1904-11).
Garza, J. J., Gantt, D. S., Van Cleave, H., Riggs, M. W. & Dehmer, G. J. Hospital disposition and long-tem follow-up of patients aged ≥ 80 years undergoing coronary artery revascularization. Am. J. Cardiol. 92, 590–592 (2003).
Gimbel, M. E. et al. Long-term follow-up after bypass surgery or coronary stenting in elderly with multivessel disease. Netherlands Heart J. 28, 467–477 (2020).
Graham, M. M. et al. Survival after coronary revascularization in the elderly. Circulation 105, 2378–2384 (2002).
Gunn, J. et al. Comparison of results of coronary artery bypass grafting versus percutaneous coronary intervention in octogenarians. Am. J. Cardiol. 110, 1125–1129 (2012).
Hara, H. et al. Five-year outcomes after coronary artery bypass grafting and percutaneous coronary intervention in octogenarians with complex coronary artery disease. Gen. Thorac. Cardiovasc. Surg. 70, 419–429 (2022).
Kamiya, M. et al. Clinical outcome and quality of life of octogenarian patients following percutaneous coronary intervention or surgical coronary revascularization. Circ. J. 71, 847–854 (2007).
Kaul, T. K., Fields, B. L., Wyatt, D. A., Jones, C. R. & Kahn, D. R. Angioplasty versus coronary artery bypass in octogenarians. Ann. Thorac. Surg. 58, 1419–1426 (1994).
Article CAS PubMed Google Scholar
Mick, M. J., Simpfendorfer, C., Arnold, A. Z., Piedmonte, M. & Lytle, B. W. Early and late results of coronary angioplasty and bypass in octogenarians. Am. J. Cardiol. 68, 1316–1320 (1991).
Article CAS PubMed Google Scholar
Nicolini, F. et al. Coronary artery surgery versus percutaneous coronary intervention in octogenarians: Long-term results. Ann. Thorac. Surg. 99, 567–574 (2015).
Rodes-Cabau, J. et al. Nonrandomized comparison of coronary artery bypass surgery and percutaneous coronary intervention for the treatment of unprotected left main coronary artery disease in octogenarians. Circulation 118, 2374–2381 (2008).
Sheridan, B. C. et al. Three-year outcomes of multivessel revascularization in very elderly acute coronary syndrome patients. Ann. Thorac. Surg. 89, 1889–1895 (2010).
Article PubMed PubMed Central Google Scholar
Wu, X. Y. et al. Clinical efficacy of different treatments and their impacts on the quality of life of octogenarians with coronary artery disease. Chin. Med. J. 132, 2657–2663 (2019).
Article CAS PubMed PubMed Central Google Scholar
We thank Mr. Benjamin May for his editorial assistance. We acknowledge support by the German Research Foundation Project-Nr. 512648189 and the Open Access Publication Fund of the Thueringer Universitaets- und Landesbibliothek Jena.
Open Access funding enabled and organized by Projekt DEAL. TC was funded by the Deutsche Forschungsgemeinschaft (DFG, German Research Foundation) Clinician Scientist Program OrganAge funding number 413668513, by the Deutsche Herzstiftung (DHS, German Heart Foundation) funding number S/03/23 and by the Interdisciplinary Center of Clinical Research of the Medical Faculty Jena. MPS receives support from The Thoracic Surgery Foundation (charitable arm of The Society of Thoracic Surgeons–STS) through the TSF Every Heartbeat Matters Global Structural Heart Fellowship Award for the project “Structural Heart/Minimally Invasive Cardiac Surgery”.
The following authors contributed equally: Hristo Kirov and Tulio Caldonazo.
Department of Cardiothoracic Surgery, Friedrich-Schiller-University, Jena, Germany
Hristo Kirov, Tulio Caldonazo, Leoni Lu Riedel, Alexandros Moschovas, Mahmoud Diab, Gloria Ferber & Torsten Doenst
Division of Cardiothoracic Surgery, University of North Carolina, Chapel Hill, USA
Department of Cardiothoracic Surgery, Friedrich-Schiller-University Jena, Am Klinikum 1, 07747, Jena, Germany
You can also search for this author in PubMed Google Scholar
You can also search for this author in PubMed Google Scholar
You can also search for this author in PubMed Google Scholar
You can also search for this author in PubMed Google Scholar
You can also search for this author in PubMed Google Scholar
You can also search for this author in PubMed Google Scholar
You can also search for this author in PubMed Google Scholar
You can also search for this author in PubMed Google Scholar
H.K., T.C., and T.D. designed the study. T.C. performed the literature review in the three different libraries. H.K. and T.C. selected the studies, qualified the studies according to the risk of bias, performed the data abstraction, built the tables and organized the results. P.T. and A.M. performed the statistical analyses. M.D., G.F. and T.D. analyzed the data. H.K., T.C., M.D., G.F. und T.D. wrote the manuscript. All the authors read and approved the final version of manuscript.
The authors declare no competing interests.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
Kirov, H., Caldonazo, T., Riedel, L.L. et al. Comparing outcomes between coronary artery bypass grafting and percutaneous coronary intervention in octogenarians with left main or multivessel disease. Sci Rep 13, 22323 (2023). https://doi.org/10.1038/s41598-023-49069-2
DOI: https://doi.org/10.1038/s41598-023-49069-2
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.
Scientific Reports (Sci Rep) ISSN 2045-2322 (online)
Electrode Gel For Tens Pads Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.